Spinal implant infections are among the most serious complications following spine surgery, often requiring revision procedures, extended antibiotic treatment and prolonged recovery times. Dr. Larry Davidson, an experienced specialist in spinal care, recognizes that nanocoatings offer a cutting-edge solution to minimize bacterial adhesion and reduce infection risk without compromising implant performance.
These microscopic surface treatments are changing the way spinal implants interact with their biological environment. By modifying texture, chemistry and topography at the nanoscale, nanocoatings not only inhibit bacterial growth but also support tissue healing and integration. This dual benefit makes them one of the most exciting advancements in spinal surgery in recent years.
The Challenge of Spinal Implant Infections
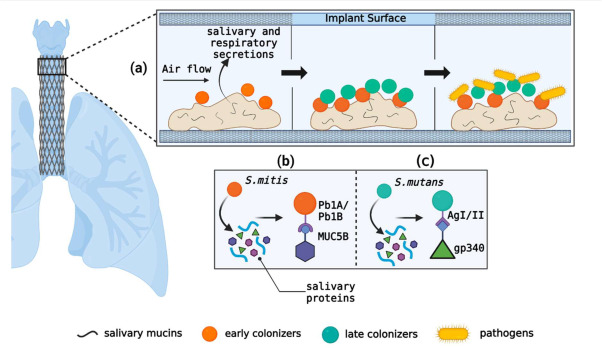
Infection after spinal surgery, while relatively rare, can lead to severe outcomes. Once bacteria attach to the surface of an implant, they can form biofilms, protective layers that shield the organisms from antibiotics and immune defenses. These infections are difficult to treat non-surgically and may require hardware removal or additional surgeries. Factors such as long operating times, patient comorbidities and compromised immunity increase the risk. Because standard implants provide a static surface that bacteria can colonize easily, innovations that actively resist infection, like nanocoatings, are crucial in high-risk cases.
What Are Nanocoatings?
Nanocoatings are ultra-thin films engineered at the nanometer scale, typically less than 100 nanometers thick. These coatings are applied to the surface of spinal implants made of titanium, PEEK or other materials to change how the implant behaves on a biological level. Even at a microscopic scale, these coatings can significantly impact how proteins, bacteria and human cells interact with the implant. Some nanocoatings are bactericidal, disrupting microbial membranes or releasing ions that kill pathogens. Others support cell adhesion and healing by creating a nanoscale surface that mimics natural tissue.
Types of Nanocoatings in Spinal Applications
There are several types of nanocoatings being used or tested for spinal implants. Silver nanoparticle (AgNP) coatings are among the most common, known for their broad-spectrum antibacterial activity. They work by releasing silver ions that interfere with bacterial respiration and DNA function. Titanium dioxide nanotubes (TiO₂) are also popular; these can be loaded with antibiotics for slow, controlled release after surgery.
Zinc oxide and copper-based nanocoatings offer alternative antimicrobial effects, while polymer-based nanocoatings can prevent protein or bacterial adhesion altogether. In some cases, hydroxyapatite nanocoatings are used not just for bone integration but also as carriers for antibacterial agents.
How Nanocoatings Prevent Infection
Nanocoatings offer several mechanisms to prevent bacterial colonization. Some work through contact killing, where the surface physically damages the bacteria upon contact. Others rely on ion release, as with silver or copper, to poison bacteria in their immediate environment. Anti-adhesive coatings are engineered to make it physically difficult for bacteria to latch onto the surface. More advanced coatings can incorporate smart-release systems, delivering antimicrobial agents only when needed, such as when a change in pH signals infection risk. These strategies help implants stay sterile and reduce the need for systemic antibiotics.
Supporting Healing Alongside Infection Control
One of the most important characteristics of effective nanocoatings is their ability to balance antibacterial action with biocompatibility. Coatings must discourage bacterial growth without interfering with human cell activity. Many modern nanocoatings are designed to support osseointegration by encouraging osteoblasts (bone-forming cells) to adhere to and grow along the implant surface. Nano topographies that mimic bone’s extracellular matrix help facilitate faster healing and stronger fusion, especially when paired with bioactive materials. As a result, nanocoatings not only protect but also promote recovery.
Dr. Larry Davidson underscores, “Emerging minimally spinal surgical techniques have certainly changed the way that we are able to perform various types of spinal fusions. All of these innovations are aimed at allowing for an improved patient outcome and overall experience.” These advancements, when combined with next-generation surface technologies like nanocoatings, reflect a broader commitment to accelerating healing while minimizing surgical risks.
Current Clinical Use and Evidence
Several nanocoated spinal implants are already in clinical use, with promising results. For instance, silver-coated devices have shown a reduction in postoperative infection rates without signs of systemic toxicity. Titanium nanotube coatings loaded with antibiotics have demonstrated success in animal studies and early human trials, showing improved bone bonding and decreased bacterial colonization.
Ongoing research is exploring how to refine these coatings for greater durability, long-term safety and broader antimicrobial protection. Regulatory interest is also growing as these coatings show favorable outcomes in spinal and orthopedic applications.
Challenges in Implementing Nanocoatings
Despite their potential, nanocoatings present some challenges. First, long-term safety must be verified, especially in coatings that release metal ions, as excessive exposure may pose risks to surrounding tissue. Second, coating durability is critical; if the layer wears off over time, its protective effects are lost.
Third, manufacturing consistency must be maintained to ensure every implant performs as expected. Lastly, cost-effectiveness is a consideration; while these innovations may reduce revision surgeries, they can also increase initial implant costs. Ongoing improvements in material science and regulatory oversight are helping address these concerns.
The Future of Smart and Responsive Nanocoatings
The next generation of nanocoatings can likely include smart functionalities that respond to environmental changes. These may include pH-sensitive coatings that release antibiotics only when infection is present or dual-function coatings that prevent both infection and inflammation. AI-assisted implant design may also help customize which nanocoating is ideal for each patient based on risk factors, comorbidities and surgical type. Researchers are also working on nanocoatings that support multi-modal healing, combining antimicrobial, osteogenic and anti-inflammatory properties in a single, multifunctional surface.
Educating Patients About Infection Prevention
As spinal implant technology advances, patients should understand what materials and features are being used in their procedures. Explaining that an implant has an infection-resistant nanocoating can increase confidence and encourage patients to participate more actively in their postoperative care. Surgeons should also emphasize that while coatings reduce risk, proper wound care, hygiene and adherence to follow-up schedules remain essential components of infection prevention.
A Microscopic Innovation with Major Benefits
Nanocoatings represent a powerful innovation in the fight against postoperative spinal infections. By modifying implant surfaces at the molecular level, they offer a proactive approach to surgical safety, protecting patients from complications while supporting healing. Nanotechnology is redefining expectations for what spinal implants can achieve. As these microscopic advancements continue to develop, they are likely to become a gold standard in surgical design, creating safer, smarter and more biologically compatible spinal solutions for the future.